Diagnosis of varicose veins
The specialist medical fields that deal with varicose veins include internal medicine, angiology, phlebology and specialised general medicine.
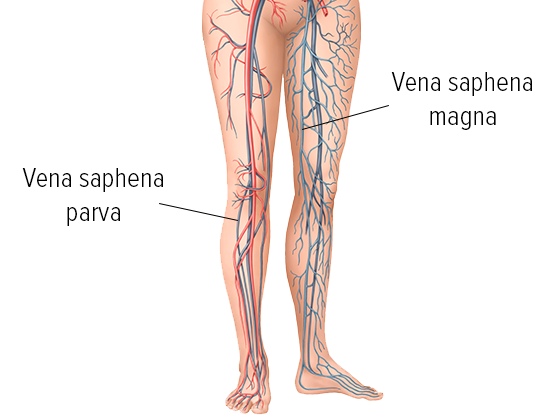
The first step of the diagnosis process is taking a medical history to clarify congenital predisposition and risk factors. This is followed by palpation and looking at the affected veins, in particular where the superficial veins connect to the deep vein system in the groin, back of the knee and lower leg. During this process, the person being treated will change positions from standing to sitting and then lying. Increased skin temperature, hardening or reddening of the skin or pressure sensitive areas can be signs of inflammation of the superficial veins. The foot pulse is taken.
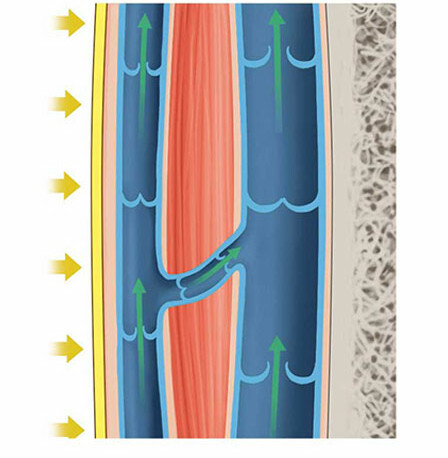
The most common diagnostic procedure in cases of varicose veins is an ultrasound examination using colour-coded duplex sonography with a Doppler ultrasound probe. These procedures are effective for detecting impairments in blood circulation, venous valves not closing fully, and for assessing the extent of vein damage. The direction of blood flow can be depicted using a colour scale.
Light reflection rheography records the pumping function of the veins, and venous occlusion plethysmography the capacity as well as the venous return. These two methods are standard practice, in particular as part of checking up on serious vascular disorders as well as before and after surgery.
Pressure measurements were common in the past. These days, they are generally replaced by modern and more reliable examination methods, including new imaging technology. X-ray examinations using contrast agent (phlebography) are rarely used now. Magnetic resonance imaging (magnetic resonance phlebography) or computer tomography based on contrast agents is used only for rare symptoms.
Laboratory examinations of individual coagulation factors can be important in cases of deep vein thrombosis, or if there is an embolism with no discernible cause.